Welcome to iGrow News, Your Source for the World of Indoor Vertical Farming
Nearly 60,000 Pounds of Frozen Raw Chicken Products Sold at Aldi and Other Stores Recalled
Serenade Foods is recalling nearly 60,000 pounds of frozen, raw, breaded and pre-browned stuffed chicken products that could be contaminated with Salmonella Enteritidis, the USDA Food Safety and Inspection Service announced Monday.
By Christina Maxouris
August 10, 2021
View this video here
(CNN) Serenade Foods is recalling nearly 60,000 pounds of frozen, raw, breaded and pre-browned stuffed chicken products that could be contaminated with Salmonella Enteritidis, the USDA Food Safety and Inspection Service announced Monday.
The products were produced on February 24 and February 25, 2021, and were shipped to distributors across the country, the service said.
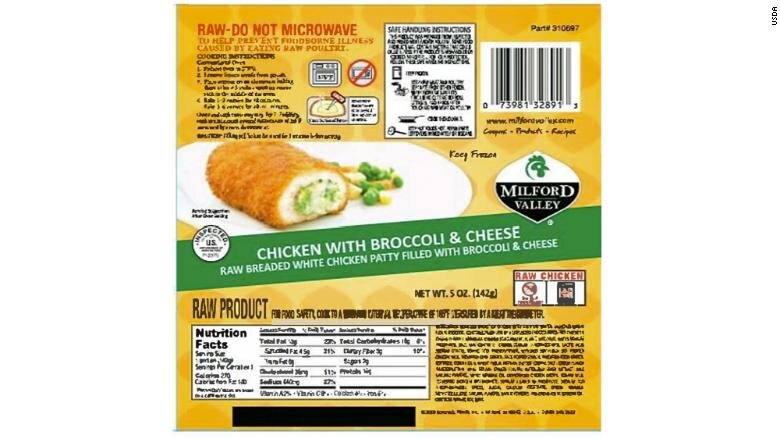
A label of one of the Serenade Foods products included in the recall
They include specific lots of the Dutch Farms Chicken with Broccoli & Cheese packages; Milford Valley Chicken with Broccoli & Cheese; Milford Valley Chicken Cordon Bleu; Kirkwood Raw Stuffed Chicken, Broccoli & Cheese; and Kirkwood Raw Stuffed Chicken Cordon Bleu, which is sold at Aldi.
The service said it was "concerned" that some of these products may be in Americans' freezers and urged consumers not to eat them.
"These products should be thrown away or returned to the place of purchase," it said.
The Service said it has been working with the US Centers for Disease Control and Prevention and other health officials to investigate an outbreak of 28 Salmonella Enteritidis illnesses across eight different states. The illnesses' timelines range from February 21 through June 28.
A second product involved in the recall
"Unopened intact packages of raw, frozen, breaded chicken stuffed with broccoli and cheese were collected from an ill person's home and tested positive for the outbreak strain of Salmonella Enteritidis," the service said. "FSIS continues to work with the CDC and state and local public health partners on this investigation."
Eating food that is contaminated with Salmonella can cause a bacterial food borne illness called salmonellosis which can cause diarrhea, abdominal cramps, and fever within 12 to 72 hours after eating the product.
"Most people recover without treatment. In some persons, however, the diarrhea may be so severe that the patient needs to be hospitalized. Older adults, infants, and persons with weakened immune systems are more likely to develop a severe illness. Individuals concerned about an illness should contact their health care provider," it said.
FDA’s Warning Shot For Leafy Greens
I hope it will serve as a call to urgent action that gets to the root of the problem of the persistent presence of dangerous E. coli in the growing environment for leafy greens and other fresh produce
On April 6, the Food and Drug Administration fired an unmistakable warning shot at the leafy greens industry. I hope it will serve as a call to urgent action that gets to the root of the problem of the persistent presence of dangerous E. coli in the growing environment for leafy greens and other fresh produce.
Carefully using the regulatory language in its produce safety rule (21 CFR 112.11) and citing the recurring nature of the E. coli hazard in the Salinas and Santa Maria growing area, FDA declared the recurring strain implicated in the 2020 outbreak to be a “reasonably foreseeable hazard,” which FDA attributed to the presence of cattle on land adjacent to growing fields.
This finding seems obvious and shouldn’t be surprising. The surprise, however, is that FDA used regulatory language to express its finding and spelled out the implications: farms covered by the FSMA produce safety rules “are required to implement science and risk-based preventive measures” to minimize the risk of serious illness or death from the E. coli hazard.
Make no mistake, however, FDA’s message is aimed not only at farms but at every entity involved in the commercial production, processing, and sale of leafy greens coming from the California Central Coast Growing Region. The message is that, without effective preventive measures, such leafy greens are in violation of federal food safety regulatory standards.
I do not anticipate FDA taking judicial action to enforce its April 6 finding, absent egregious practices or clear negligence in a particular leafy green growing situation. I do see, however, a heightened sense of urgency at FDA and frustration that efforts to date have not solved the leafy greens safety problem. I share that frustration.
Fifteen years ago, the disastrous spinach outbreak caused by E. coli O157:H7 was linked by the Centers for Disease Control and Prevention (CDC) to run-off from nearby grazing land. Since then, we’ve had outbreak after outbreak associated with E. coli in leafy greens and other fresh produce. And the outbreaks are just the tip of the public health iceberg. The federal government estimates that 60 percent of all food-related E. coli O157:H7 illnesses are associated with fresh produce. The vast majority of these illnesses are not part of an identified outbreak.
The E. coli outbreaks and illnesses persist despite a lot of hard work by a lot of people in the leafy greens industry, researchers, the California Department of Food and Agriculture (CDFA), the FDA and its federal partners. Stop Foodborne Illness, the organization of illness victims and their families whose board I co-chair, works with the California LGMA on the common cause of strengthening food safety culture in the leafy green industry. We also advise the Leafy Greens Safety Coalition, a group of leading retailers working to strengthen safety practices. I have participated in the California Agricultural Neighbors Workgroup convened by CDFA Secretary Karen Ross. So, I know serious people are at work on the problem.
What then is the urgent call to action? What do consumers expect of the leafy greens industry, especially those individuals and families who know first-hand the devastating human impact E. coli infections can have? What does the public health demand?
At one level, the answer to all three questions is the same. The leafy greens industry and all those across the leafy greens supply chain and in government should be doing urgently everything they reasonably can to minimize the now well-known risk posed by E. coli O157:H7. According to FDA, the law requires no less. Certainly, this includes prevention measures within the leafy greens production system, such as strict implementation of rigorous water quality and irrigation standards, improved compost management, sanitation of harvesting equipment, and pre-harvest test-and-hold programs.
But the prevention strategy must go deeper. Modern food safety best practices dictate that prevention should begin at the root of the problem. As long as leafy greens are grown outdoors in the vicinity of cattle operations, I believe the food safety problem will persist until the shedding by cattle and the release of dangerous E. coli into the environment is minimized at its source. Effective vaccines are available. Changed feeding practices have promise. Perhaps containment measures can reduce risk.
The experts need to determine what combination of measures works best, but it is clear that no responsible food manufacturer would today deem it acceptable to produce food in an environment in which dangerous bacteria are being released or are present on a sustained basis. The same principle should apply to leafy greens and other fresh produce grown outdoors.
The important difference, of course, is that the leafy greens producer has no direct control over the source of the hazard. And the cattle producer isn’t responsible for where leafy greens are grown. That is why FDA Deputy Commissioner Frank Yiannas calls for “industry leadership and collaboration among growers, processors, retailers, state partners and the broader agricultural community,” including cattle producers.
I am glad FDA is sounding the alarm, but I know from experience that the kind of leadership and collaboration that is urgently needed is easier said than done in an industry and government structure that is notoriously fragmented and often works in silos. And the obstacles to solving the problem are not just technical. They include the need for creative solutions on such matters as who pays for interventions needed in cattle production to make leafy greens safe.
But too much is at stake for all concerned to let such obstacles stand in the way. Now is the time for leaders from all across the commercial value chain and government to act together, with greater urgency, to get to the root of the problem and prevent it.
Mike Taylor
About the author: Mike Taylor is co-chair of the board of the non-profit consumer advocacy group Stop Foodborne Illness, which is a 25-year-old group supporting and representing foodborne illness victims and their families in efforts to keep other people from getting sick. Before that Taylor served as FDA’s Deputy Commissioner for Foods and Veterinary Medicine from 2010 to mid-2016. His first tour in government began as a staff attorney at FDA, where he worked on seafood safety and nutrition labels. Later Taylor worked for USDA’s Food Safety and Inspection Service, where he became acting under secretary for food safety. Taylor was the government official who, after the deadly 1992-93 Jack in the Box hamburger outbreak, ruled that the pathogen E. coli O157:H7 is an adulterant in meat. Taylor also practiced law in the private sector.
(To sign up for a free subscription to Food Safety News, click here.)
FDA: E. coli Outbreak Investigation Closes; No Specific Source Found
Epidemiological and traceback investigations did not determine a specific leafy green, brand, or supplier, but the E. coli strain is genetically related to a strain linked to a fall 2019 outbreak from romaine lettuce
By CHRIS KOGER January 28, 2021
(Courtesy FDA)
An investigation into a fall 2020 outbreak of E. coli linked to leafy greens found cattle manure with the same strain about a mile from a field in California’s Salinas Valley, but the pathogen was not detected on any leafy greens or farms they were grown on.
The Food and Drug Administration released an update on its investigation on the outbreak on Jan. 27, and a full report will be released later. Forty people became sick in the outbreak, and half of them were hospitalized.
“Although the investigation has been unable to identify a specific type of leafy green at the heart of this outbreak, it is clear that this is yet another outbreak tied to leafy greens,” Frank Yiannas, the FDA’s deputy commissioner for food policy and response said in a news release on the agency’s findings.
Epidemiological and traceback investigations did not determine a specific leafy green, brand, or supplier, but the E. coli strain is genetically related to a strain linked to a fall 2019 outbreak from romaine lettuce.
Investigators from the FDA and other agencies visited dozens of farms in the Salinas Valley to collect samples. They also collected samples in adjacent areas, testing animal feces, compost, and water, according to the FDA. The cattle manure that yielded the positive test result was found on a roadside, uphill from where “leafy greens or other food identified on the traceback investigation were grown,” according to the FDA release.
“This finding draws our attention once again to the role that cattle grazing on agricultural lands near leafy greens fields could have on increasing the risk of produce contamination, where contamination could be spread by water, wind or other means,” Yiannas said in the release.
The FDA continues to recommend that growers assess and mitigate risks from areas adjacent to their fields, particularly in the vicinity of cattle operations, he said. That is a specific goal of the FDA’s Leafy Greens Action Plan, released in March, he said.
Yiannas said the FDA’s final report on the outbreak will include recommendations “shaped by these findings.”
FDA Releases Protocol on The Treatment of Agricultural Water
The Food and Drug Administration has a new protocol for the development and registration of treatments for water used on crops before harvest
July 30, 2020
The Food and Drug Administration has a new protocol for the development and registration of treatments for water used on crops before harvest.
( Courtesy FDA )
The FDA announced the protocol during a July 30 web seminar on its 2020 Leafy Greens STEC Action Plan, referring to Shiga toxin-producing E. coli, which has caused 40 foodborne illness outbreaks from 2009 and 2018, according to the federal agency.
The FDA and Environmental Protection Agency worked on the protocol.“
This new protocol is a huge milestone for produce safety and for the Leafy Green Action Plan released by the FDA earlier this year,” Frank Yiannas, FDA deputy commissioner for food policy and response, said in the agency’s announcement. “Working together, the FDA and EPA have supported the development of this protocol that may ultimately help farmers address contamination issues in their water sources and protect consumers from foodborne illness.”
There are no registered antimicrobial treatment products authorized to control “microorganisms of public health significance” for agricultural fields, or treatment of irrigation water systems or ponds, according to an FDA news release.
The protocol is intended to help companies develop data on the effectiveness of their products on pathogens including E. coli and salmonella in preharvest agricultural water.“
Teams of FDA experts have been working collaboratively with partners in the public and private sectors to help protect agricultural water from the many ways it can be contaminated in the environment or from unsanitary practices on a farm,” according to the FDA announcement. “This effort has included hundreds of farm visits over the past few years.”
The FDA plans to propose a rule late this year that would revise agricultural water requirements in the Food Safety Modernization Act’s Produce Safety Rule, according to the announcement.
FDA Suspends Inspections In Foreign Countries Due To Coronavirus
The FDA announced the decision on March 10 with a statement from Commissioner Stephan Hahn. Customs and Border Protection officers will continue to examine produce arriving at U.S. points of entry, but food safety inspections at foreign facilities are postponed until April, according to the FDA.“
March 11, 2020
The Food and Drug Administration has halted most inspections of food facilities outside of the U.S. through April, as travel restrictions increase in response to the COVID-19 outbreak.
The FDA announced the decision on March 10 with a statement from Commissioner Stephan Hahn. Customs and Border Protection officers will continue to examine produce arriving at U.S. points of entry, but food safety inspections at foreign facilities are postponed until April, according to the FDA.“
Mission-critical” inspections will be decided on a case-by-case basis.
The decision also affects on-site inspections at foreign drug and medical device manufacturers.
The FDA is employing interim measures, including Denial of imports;
Examination and sampling of products at ports of entry;
Reviewing a company’s compliance history;
Using information-sharing agreements with foreign governments; and
Requesting records “in advance of or in lieu of” on-site inspection.“
The FDA will continue working with U.S. Customs and Border Protection to target products intended for importation into the U.S. that violate applicable legal requirements for FDA-regulated products, which may come from a variety of sources, such as first-time importers unfamiliar with regulatory requirements or repeat offenders trying to skirt the law,” Hahn wrote in the statement.
The FDA uses the Predictive Risk-based Evaluation for Dynamic Import Compliance Targeting (PREDICT) system for risk-based import screening to focus on high-risk imports. The agency also checks for “port shopping” or cargo diversions, according to Hahn.
The FDA continues to monitor the outbreak’s effect on operations.“
As this remains a dynamic situation, we will continue to assess and calibrate our approach as needed to help advance federal response efforts in the fight against this outbreak,” according to Hahn’s statement.
Related stories:
Coronavirus gives ‘body blow’ to exporters, worries consumers
United Fresh discusses coronavirus, product trends at FPFC event
Is It Safe To Eat Romaine Lettuce From Salinas Again? CDC Says E. coli Scare “Appears To Be Over”
The Centers for Disease Control and Prevention said in an updated food safety report that it is “no longer advising that people avoid romaine lettuce from the Salinas Valley growing region in California.”
By Kelly Tyko, USA TodayJan 15, 2020
After nearly three months, the romaine lettuce outbreak “appears to be over,” federal health officials announced Wednesday.
The Centers for Disease Control and Prevention said in an updated food safety report that it is “no longer advising that people avoid romaine lettuce from the Salinas Valley growing region in California.”
Since Nov. 22, the CDC and the Food and Drug Administration have told consumers to avoid the lettuce from California as they investigated multistate E. coli outbreaks.
A total of 167 people from 27 states were infected with the outbreak strain of E. coli O157:H7, the CDC said Wednesday.
A total of 85 hospitalizations were reported, and 15 people developed hemolytic uremic syndrome, a type of kidney failure. No deaths were reported, the CDC said.
The ages of those who fell ill ranged from infancy to 89 years old, with a median age of 27. Several people in Canada also may have been affected.
The CDC was able to interview 113 people who fell ill, with 83 percent of them saying they’d eaten romaine lettuce, much higher than a survey of healthy adults.
Frank Yiannas, FDA deputy commissioner for food policy and response, said in a statement that the investigation is ongoing and they are “doing everything possible to find the source or sources of contamination.”
“The investigation into how this contamination occurred is important, so romaine growers can implement measures that will prevent future contamination and illnesses,” Yiannas said.
This outbreak was caused by the same strain of “Shiga toxin-producing” E. coli that caused outbreaks linked to leafy greens in 2017 and to romaine lettuce in 2018, the CDC said. The Shiga toxin can cause severe stomach cramps, diarrhea that is often bloody and vomiting. Severe dehydration can result.
Contributing: Joe Szydlowski, Salinas Californian
Which Fish Has The Highest And Lowest Mercury Levels?
Fish is one of the best sources of protein, omega-3 fatty acids, and other nutrients including iron, potassium and B vitamins. Unfortunately, much of our world's seafood supply is contaminated with high levels of toxic mercury. (You can thank industrial runoff for that!)
MAYA FELLER, MS, RD, CDN
UPDATED ON JULY 5, 2019
Fish is one of the best sources of protein, omega-3 fatty acids, and other nutrients including iron, potassium and B vitamins. Unfortunately, much of our world's seafood supply is contaminated with high levels of toxic mercury. (You can thank industrial runoff for that!)
What Is Mercury?
So, we know that mercury isn't exactly good for you. But before we get into why, let's begin by answering the question, what is mercury?
Methylmercury — the most poisonous among the mercury compounds — is formed when inorganic mercury is dissolved in both freshwater and seawater. The cascade begins when this toxic compound becomes embedded into the food chain after being consumed by phytoplankton, a single-celled alga, which is then consumed by smaller animals.
This is particularly problematic because the smaller fish shed nonorganic mercury as waste, while methyl mercury is retained. As we move up the food chain, smaller fish are consumed by larger fish and those fish are consumed by even bigger fish — all retaining methyl mercury until it makes its way to humans in a process called biomagnification.
Why Is Mercury Bad For Us?
The concern around mercury toxicity is not solely limited to just developing nations — the effects are far-reaching and relevant for all people around the globe. A November 2012 study in the Journal of Preventive Medicine & Public Health has shown that high levels of mercury can damage the central nervous system and pose deleterious effects on the brain — specifically, decreased attention and memory as well as symptoms such as trembling and impaired vision.
And, a July 2012 study in the Journal of Biomedicine and Biotechnology linked high mercury exposure to an increased risk of heart disease. Researchers think this is due to mercury's ability to increase the production of free radicals while reducing antioxidants in the body, which results in oxidative stress.
How Can You Avoid Eating Too Much Mercury?
In general, a good rule of thumb when it comes to mercury content is to consider the size of the fish. Smaller fish such as salmon, scallops, sardines and shrimp contain less mercury than their larger predators such as bigeye tuna and swordfish.
The standard serving size of fish is about four ounces — or the size of the palm of your hand, according to the U.S. Food & Drug Administration. Use the following guide to help you choose fish with the lowest mercury levels and find out how often you should eat other popular types of seafood.
Seafood With the Lowest Mercury Content
Eat 2 to 3 times a week:
Anchovies
Atlantic croaker
Atlantic and Pacific chub mackerels
Black sea bass
Butterfish
Catfish
Clams
Cod
Crab
Crawfish
Flounder
Freshwater trout
Haddock
Hake
Herring
American spiny lobster
Mullet
Oyster
Perch
Pickerel
Plaice
Pollock
Salmon
Sardines
Scallops
Shad
Shrimp
Skate
Smelt
Sole
Squid (calamari)
Tilapia
Tuna (canned light, skipjack)
Whitefish
Whiting
Fish With Moderate Levels of Mercury
Eat 1 serving a week:
Bluefish
Buffalofish
Carp
Chilean sea bass
Grouper
Halibut
Mahi mahi
Monkfish
Rockfish
Sablefish
Sheepshead
Snapper
Spanish mackerel
Striped bass
Tilefish
Tuna (albacore/white tuna, canned or fresh/frozen)
Yellowfin tuna
Weakfish/seatrout
White croaker/Pacific croaker
Fish With the Highest Mercury Levels
Fish to avoid:
Bigeye tuna
King mackerel
Marlin
Orange roughy
Shark
Swordfish
Tilefish (Gulf of Mexico)
When making choices about seafood, it is important to be an informed consumer who understands the differences between the varieties as well as sourcing of their fish. Seafood, in moderation, can and should be a part of a balanced eating plan thanks to the anti-inflammatory omega-3s and lean protein in fish. In fact, the American Heart Association recommends eating at least two 3.5-ounce servings of fish a week — so choose wisely!
Lead Image: (Image: Getty Images/Boris SV)
BREAKING NEWS: MINNESOTA - Bad Basil Sickens Some In Twin Ports
Imported basil sickened nine people at two restaurants in the Twin Ports in June as part of a multi-state cyclospora illness outbreak, according to the Minnesota Department of Health
No Ongoing Risk, Health Department Says
Written By: News Tribune | Jul 26th 2019
Imported basil sickened nine people at two restaurants in the Twin Ports in June as part of a multi-state cyclospora illness outbreak, according to the Minnesota Department of Health.
The department said there were four lab-confirmed cases from Outback Steakhouse in Hermantown and five cases from meals catered by Duluth Grill at a Duluth conference. There were 26 confirmed cases at City Market in Rochester. None of the Minnesota cases required hospitalization.
"It's important to note that the illnesses are the result of contaminated imported food product, not anything the restaurants did or did not do," department spokesman Doug Schultz said. "We have no evidence of any ongoing risk at the restaurants involved."
The contaminated basil was exported from Mexico to the United States by Siga Logistics de RL de CV, according to the Food and Drug Administration; the company has agreed to a voluntary recall.
There have been four hospitalizations out of 132 total illnesses in 11 states since the cyclospora outbreak was first reported in late June, according to the FDA. The last reported illness came on July 9.
Cyclospora is a parasite that is transmitted when infected feces contaminated food or water and can take about a week from infection to sickness; symptoms include diarrhea, loss of appetite, nausea and fatigue.
Lead Photo: Basil seedlings. Credit: extension.umn.edu
Manufacturer Recalls Salads, Sandwiches Sold At Target, Fresh Market Due To Health Risk
The manufacturer of some salads and sandwiches sold at Target and The Fresh Market has issued a recall due to potential listeria contamination, according to the U.S. Food and Drug Administration
The manufacturer of some salads and sandwiches sold at Target and The Fresh Market has issued a recall due to potential listeria contamination, according to the U.S. Food and Drug Administration.
Elevation Foods is voluntarily recalling some containers of Archer Farms-brand egg salad; Freskëtbrand egg salad, tuna salad, and Thai lobster salad; and Archer Farms-brand deviled egg sandwiches produced on June 18, 2019.
On its website, The Fresh Market says its Thai lobster salad that's sold both prepackaged and by the pound at its self-serve seafood is included in the recall.
According to Elevation Foods, fewer than 1,087 cases of product were shipped to retailer warehouses throughout the United States.
Archer Farms Egg Salad is one of several salads included in a voluntary recall by Elevation Foods. (Photo: Provided)
To see if you have a product that's included in the recall, check the “use by” date printed on the side of the container and the lot number. The FDA website lists the following items as impacted by the recall:
Archer Farms-brand Egg Salad packaged in a 12-ounce clear, square plastic container, Lot Number W1906042A, Use By 12AUG2019 (printed on the side of each container) UPC 085239018682, distributed nationwide;
Freskët-brand Egg Salad packaged in a 32-ounce clear, square plastic container, Lot Number W1906042, Use By 12AUG2019A (printed on the side of each container;
Freskët-brand Tuna Salad packaged in a 5-pound white, round plastic container, Lot Number W1906054, Use By 02AUG2019A (printed on the side of each container;
Freskët-brand Thai Lobster Salad packaged in a 5-pound white, round plastic container, Lot Number W1906041, Use By 02AUG2019A (printed on the side of each container);
Archer Farms Deviled Egg Sandwich Half Sandwich with Bacon, UPC 220505000002, distributed nationwide;
Archer Farms Deviled Egg Sandwich on Multigrain, UPC 498780203566, distributed nationwide.
No illnesses have been reported, but listeria monocytogenes can cause serious and sometimes fatal infections in young children, frail or elderly people, and others with weakened immune systems, according to the FDA.
Fresket Thai Lobster Salad is one of several salads included in a voluntary recall by Elevation Foods. (Photo: Provided)
In otherwise healthy people, listeria monocytogenes can cause short-term symptoms such as high fever, severe headache, stiffness, nausea, abdominal pain, and diarrhea, according to the FDA. Listeria infection can cause miscarriages and stillbirths among pregnant women.
Elevation Foods identified the problem with the products after receiving positive test results for three containers of affected egg salad which were sampled and tested by the Florida Department of Agriculture and Consumer Services, according to the FDA website. Elevation Foods is continuing to investigate potential sources of the problem.
Consumers who have purchased any of the recalled products are urged to return them to the place of purchase for a full refund. Consumers with questions can call 866-761-9566 at any time.
Archer Farms Products Recalled Due To Possible Listeria Contamination
Some Archer Farms products are being recalled due to a possible Listeria contamination. Elevation Foods announced Friday that they are recalling containers of Archer Farms egg salad and deviled egg sandwiches
July 20, 2019
Several Freskët-Brand Products Also Affected By Recall
NEW YORK (CBSNewYork) — Some Archer Farms products are being recalled due to a possible Listeria contamination.
Elevation Foods announced Friday that they are recalling containers of Archer Farms egg salad and deviled egg sandwiches.
Elevation Foods recalled containers of Archer Farms egg salad and deviled egg sandwiches. in July 2019. (Credit: FDA)
The following products are affected by the recall:
Archer Farms-brand Egg Salad packaged in a 12-ounce clear, square plastic container, Lot Number W1906042A, Use By 12AUG2019 (printed on the side of each container) UPC 085239018682
Archer Farms Deviled Egg Sandwich Half Sandwich with Bacon, UPC 220505000002
Archer Farms Deviled Egg Sandwich on Multigrain, UPC 498780203566
All of the affected Archer Farms products were distributed nationwide.
The following Freskët-brand products are also being recalled:
Freskët-brand Egg Salad packaged in a 32-ounce clear, square plastic container, Lot Number W1906042, Use By 12AUG2019A (printed on the side of each container
Freskët-brand Tuna Salad packaged in a 5-pound white, round plastic container, Lot Number W1906054, Use By 02AUG2019A (printed on the side of each container
Freskët-brand Thai Lobster Salad packaged in a 5-pound white, round plastic container, Lot Number W1906041, Use By 02AUG2019A (printed on the side of each container)
The recall does not say where the Freskët-brand products were distributed.
No illnesses have been reported at this time.
According to the Food and Drug Administration, fewer than 1,087 cases of the products have been shipped to retailer warehouses throughout the United States.
Elevation Foods recalled containers of Archer Farms egg salad and deviled egg sandwiches. in July 2019. (Credit: FDA)
Listeria monocytogenes can cause serious and sometimes fatal infections in young children, elderly people and those with weakened immune systems. Symptoms include high fever, severe headaches, stiffness, nausea, abdominal pain and diarrhea.
Anyone who bought a recalled product should return it for a full refund.
Anyone with questions can call 866-761-9566.
Visit fda.gov for more information on this recall.
Filed Under:Archer Farms, listeria, Recall
Many Unanswered Questions, Concerns About CBD Products, Says FDA Acting Chief At First Public Hearing
The acting head of the Food and Drug Administration launched the agency’s first hearing on CBD products Friday with a laundry of list of questions about cannabidiol, better known as CBD, which is already being sold in pills, tinctures, skin lotions, sodas and dog food
You can buy CBD in oils, supplements, soda, even dog food. But most of them violates federal food and drug regulations, prompting concerns over safety and deceptive marketing.
A jar of CBD gummy candies at The Cannabis World Congress & Business Exposition trade show in New York City. REUTERS/Mike Segar (Mike Segar/Reuters)
By William Wan
May 31, 2019
The acting head of the Food and Drug Administration launched the agency’s first hearing on CBD products Friday with a laundry of list of questions about cannabidiol, better known as CBD, which is already being sold in pills, tinctures, skin lotions, sodas and dog food.
How much of the cannabis extract is safe to consume daily, he asked at the jam-packed, all-day hearing at FDA headquarters in Silver Spring. How will it interact with other drugs? What if a consumer is pregnant? What is CBD’s effect on children? What happens if someone takes it over the course of years?
Acting Commissioner Norman “Ned” Sharpless said answers to most of those questions are still unknown despite the popularity of many CBD products.
“There are important reasons to generally prohibit putting drugs in the food supply,” Sharpless said. And cannabis extracts like CBD “are no exception.”
During the 10 hours of testimony that followed, hemp growers, start-up businesses, academic researchers and consumer advocates argued about how FDA should regulate the already booming CBD industry. Some demanded strict oversight. Others — especially companies with millions at stake — lobbied for looser regulation.
But the common theme among them all: FDA needs to figure out its rules sooner, rather than later.
Even though FDA’s regulations make adding CBD to food and supplements illegal, the CBD industry has exploded in recent years with thousands of unproven products flooding the market. Companies have trumpeted the compound’s alleged health benefits — claiming it can reduce anxiety, pain and insomnia and treat conditions from Parkinson’s disease to cancer. But almost all such claims lack rigorous scientific proof, prompting concern among health officials and scientists about safety and deceptive marketing.
Without clearly defined regulations, no one knows for sure how much CBD is in products available on the market, or how safely the chemical compound is being manufactured and incorporated into them.
“It’s a wild West kind of environment right now,” said Yasmin Hurd, a psychiatry professor at the Icahn School of Medicine at Mount Sinai in New York City, who has researched CBD for almost 10 years. “I’m inundated every day with patients wanting to know how much CBD they should take, which ones to buy. But we don’t know what’s in the stuff now being sold. . . . We’ve had this explosion without guidance to the public or regulation.”
How the FDA will choose to regulate the industry and how long it will need to figure that out remain unclear. Those prospective regulations have become a fierce battleground: More than 400 people and groups applied for a chance to speak at Friday’s hearing, with roughly 120 speaking slots parsed out.
CBD can be derived from the marijuana plant or hemp. Congress in December legalized hemp as part of the Farm Bill, clearing the way for industrial production of the nonintoxicating compound from that plant. But the FDA quickly made it clear to companies that while hemp was legal, CBD extract remained under government regulation. In recent months, the agency has sent warning letters to some companies that it said were “illegally selling CBD products that claimed to prevent, diagnose, treat, or cure serious diseases, such as cancer.”
Billions are at stake in how the FDA decides to regulate the compound, with business analysts projecting the industry could grow to be worth as much as $22 billion in the next five years.
Market research firm New Frontier Data estimated that sales of CBD products in the United States more than tripled between 2014 and 2017, to $367 million.
Retailers like CVS and Walgreens have announced plans to sell CBD lotions and creams. Food and beverage companies have eagerly jumped in, too, with burger chain Carl’s Jr. selling CBD-infused burgers.
At Friday’s hearing, hemp growers argued that the CBD market represented thousands of jobs and a booming source of growth for the economy. CBD retailers relayed anecdotal evidence of patients who found relief to longstanding medical problems in their products.
Health advocates spoke equally passionately about the dangers posed by an unfettered CBD market.
So far, the agency has approved only one CBD-based drug, Epidiolex, which treats severe forms of childhood epilepsy.
In a phone interview, Orrin Devinsky, a New York University researcher who helped develop the drug, said the government’s haphazard approach has been frustrating to scientists trying to help suffering patients.
“You have researchers having to struggle through enormous expense and obstacles to study CBD,” he said. “At the same time, you can walk down to your neighborhood bodega and buy a CBD soda off the shelf. The nation and marketplace are in a horribly confused state.”
So far, treating epilepsy is the only application for CBD supported by rigorous scientific data, Devinsky said. Though less rigorous, some promising findings have emerged for CBD’s possible effect on anxiety and inflammation.
“The thing we worry about is someone with cancer forgoing real treatment like chemo and taking CBD instead,” said Devinsky, a neurology professor at NYU.
At Friday’s hearing, scientists and consumer advocates also warned that for the thousands of CBD products being sold, there is little data to guide dosage levels, expiration dates, and manufacturing protocols to make sure they don’t also contain other elements like tetrahydrocannabinol, or THC, the main psychoactive component in marijuana, which has been found in some CBD products.
Whatever the FDA decides, many in the industry are pressing for it to move quickly.
“I’ve talked to beverage companies and they want to get into this space, but they are not interested in just throwing themselves headlong into an area without science and engagement with regulators,” said Coleen Klasmeier, a former FDA staff lawyer and now partner at law firm Sidley Austin.
“For years now, the agency’s position has been just to throw up their hands and say it’s a confusing issue,” said Daniel Fabricant, a former FDA official overseeing dietary supplements, who is now chief executive of the Natural Products Association representing the supplement industry.
In addition to Friday’s hearing, the FDA has set a deadline of July 2 for written comments on the issue. It also convened a working group led by Deputy Commissioner Amy Abernethy to explore ways CBD products might be sold legally, the impact of such products on public health, and whether new FDA rules or congressional legislation may be needed.
In a string of tweets on Friday, Abernerthy summed up main points she and FDA officials were hearing over and over at the meeting: “Key questions about product safety need to be addressed. Data are needed to determine safety thresholds for CBD...There are both positive supporters of cannabis-cannabis derived products including CBD and also concerned citizens worried that widely available products can be harmful.”
Statement From FDA on Investigation of November '18 Outbreak of E. coli In Romaine Lettuce
The U.S. Food and Drug Administration and the U.S. Centers for Disease Control and Prevention acted quickly to protect consumers from an emerging outbreak of E. coli O157:H7 linked to romaine lettuce by issuing a public warning this past November and recommending that industry and retailers voluntarily remove the product from the market. It was critical to provide this advice because it was believed that contaminated produce was still in the food supply at a time when Americans were preparing meals to celebrate Thanksgiving. By removing potentially contaminated products from the market, health officials and industry were able to reduce additional illnesses.
Evidence at the beginning of this outbreak showed that the genetic fingerprint of the pathogen obtained from patients impacted by the 2018 outbreak was similar to the strains associated with an outbreak previously linked to leafy greens in 2017. With help from this historic information, our staff worked quickly to initiate traceback from points of sale through the supply chain ultimately to the farms where the romaine could have been grown. Investigators were able to narrow down the growing region to California based on trends in the industry. Moreover, the supply chain pointed to specific California counties.
The traceback investigation identified multiple farms that may have been implicated in this outbreak. These farms became the focus of further evaluation. The FDA led a team of experienced federal and state investigators who were tasked with taking samples and inspecting these farms to try and find out where and how this outbreak happened. They collected samples of soil, animal feces, fertilizer, agricultural water and reservoir sediment. The CDC was able to find one positive match to the outbreak strain in the sediment of an on-farm water reservoir, used for irrigation, in Santa Maria, Calif.
The investigation teams made numerous visits to leafy greens farms in various counties and growing regions of California identified through traceback. The outbreak strain of E. coli O157:H7 was not detected in any other samples collected during this investigation. On December 17, 2018, the farm with the positive match to the outbreak strain in the sediment issued a recall of romaine lettuce and other products -- including red leaf lettuce, green leaf lettuce and cauliflower -- that may have also been contaminated due to use of agricultural water from the on-farm reservoir.
Given the critical nature of these activities, during the partial lapse in funding, the FDA and CDC continued work on this investigation. Thanks to this continued effort during the partial funding lapse, we were able to declare the outbreak over – just over two months after it was first announced – once we were confident that contaminated product could no longer be available for purchase and there were no new illnesses linked to romaine from the implicated California growing areas. Even though the outbreak was declared over, the FDA’s investigation continued. We wanted to understand the factors that allowed this outbreak to happen and provide information to help prevent similar outbreaks from occurring again.
Today, we’re announcing the findings of this investigation and our best hypotheses as to how this contamination could have occurred. In the case of the one farm with a positive sample previously referenced, the FDA believes that the most likely way romaine lettuce on a specific ranch on this farm became contaminated was from the use of water from this reservoir as agricultural water. It is believed that this water came into contact with the harvested portion of the romaine lettuce, since the outbreak strain of E. coli O157:H7 was found in sediment from the reservoir and in no other sampled locations. The water from the reservoir doesn’t explain how lettuce grown on other ranches or farms identified by traceback may have been contaminated. So, this one farm cannot explain the entire outbreak.
As part of our investigation, we determined that the farm had a procedure in place to collect and test reservoir agricultural water for generic E. coli and to treat the agricultural water with a sanitizer before use. However, the investigation team noted the verification procedure records did not document that sufficient sanitizer was present to adequately reduce any pathogens present in the water when this water was used for direct contact with romaine lettuce at harvest, during postharvest handling, and to wash/rinse harvest equipment food contact surfaces. It’s important to note that the farm reported that it did not use water from the reservoir for the dilution of crop protection chemicals. It also remains uncertain how the outbreak strain of E. coli O157:H7 was introduced into their on-farm water reservoir.
The finding of the outbreak strain in the sediment of the water reservoir is significant, as studies have shown that generic E. coli can survive in sediments much longer than in the overlying water. It’s possible that the outbreak strain may have been present in the on-farm water reservoir for some months or even years before the investigation team collected the positive sample. It is also possible that the outbreak strain may have been repeatedly introduced into the reservoir from an unknown source.
The teams did find evidence of extensive wild animal activity, including waterfowl, rodents, coyotes, etc., and animal burrows near the contaminated reservoir. This likely warrants consideration as a possible source of the human pathogen found in the on-farm water reservoir. It is another factor that we will work with the farm to address. Additionally, adjacent land use including the use of soil amendments, or for animal grazing on nearby land, may have had the potential to be contributing factors.
As explained in the Environmental Assessment of Factors Potentially Contributing to the Contamination of Romaine Lettuce Implicated in a Multi-State Outbreak of E. coli O157:H7, which provides the findings of the unrelated spring 2018 investigation into contamination that originated in the Yuma growing region, food safety problems related to raw whole and fresh-cut (e.g. bagged salad) leafy greens are a longstanding issue. The FDA and CDC identified 29 foodborne illness outbreaks of Shiga-toxin producing E. coli (STEC) with a confirmed or suspected link to leafy greens in the United States between 2009 and 2017. STEC contamination of leafy greens has been identified by past investigations, traceback, observation and sample collection results as most likely to occur in the farm environment.
To help ensure that leafy greens are safe and mitigate problems that might occur, it’s important to understand where leafy greens are grown and harvested and not simply the location of the business entity that shipped or processed the produce. It’s also important to be able to determine which farms and growing regions are responsible for supplying the contaminated product and the time frame when product was supplied. This information is crucial to the development of accurate public health messages to both protect consumers from exposure and empower retailers and consumers to take appropriate actions.
The FDA continues to recommend that leafy green growers, buyer/shippers and retailers be able to trace product back to the specific source in real time and make information about the source, such as harvest date and standardized growing regions, readily available for consumers on either packaging or point of sale signs, or by other means. We’re pleased to see many companies in the leafy green industry take voluntary steps to quickly respond to our previous recommendations. We believe this is the best approach to be able to inform consumers should there be any future risks to public health. Our first goal is working with federal, state and industry partners on implementing best practices to try and prevent these outbreaks in the first place. But when outbreaks occur, without the ability to identify the growing region or specific suppliers of suspected shipments, the public messages issued by the FDA and other public health partners during recalls or outbreaks will continue to be -- out of necessity -- broad and likely to include farms and growing regions that may not be responsible for the contamination. We know more needs to be done and there is a shared sense of urgency around these efforts.
The FDA recommendations based on this investigation are similar to, and reinforce, the changes recommended for the leafy green industry in the Yuma environmental assessment. We continue to strongly recommend that all segments of the leafy greens industry thoroughly review current operations, procedures, policies and practices taking into consideration the findings of this investigation report, the FSMA Produce Safety Rule, the FSMA Preventive Controls for Human Foods Rule and other relevant FSMA regulations. Other available science-based information relevant to the reduction or elimination of human pathogens on leafy greens should also be considered. In addition, industry should make the necessary modifications to operations, procedures, policies and practices to ensure safe products for consumers and minimize the likelihood of similar outbreaks in the future.
We’ll continue to work with industry to explore better ways to assure quick, accurate and easy access to key traceability information. The FDA believes that widespread industry adoption of existing and emerging technologies, which can be used to trace product from the field to the consumer in real time, is a critical piece of our ability to protect the public. In addition, the agency has already started special, microbiological surveillance sampling assignments for romaine lettuce that is grown for distribution throughout the country. If samples are found to be contaminated, the FDA will follow-up with the responsible farms and firms to assure that they remove contaminated products from the market. The agency will also work with responsible farms to determine issues and identify steps they can put in place to prevent contamination in the future.
Advancing the safety of fresh leafy greens requires ongoing collaboration. We urge all segments of this industry, from farm to table, and our government partners to review the findings of our investigation and make necessary changes. We recognize and appreciate the efforts that the leafy greens industry has taken to date. But together, we also know more must be done on all fronts to help prevent future foodborne illness outbreaks. We remain committed to further strengthening the FDA’s food program and applying our food safety expertise as we work to better safeguard the U.S. food supply.
Despite Hemp Legalization, FDA Will Still Consider CBD Products Largely Illegal
FDA maintains hemp oil is a drug ingredient, and requires approval for products.
Published: Dec 23, 2018
Reuters
By ASSOCIATEDPRESS
SEATTLE — The hemp industry still has work ahead to win legal status for hemp-derived cannabidiol, or CBD oil, as an ingredient in food or dietary supplements despite the big farm bill President Donald Trump signed last week designating hemp as an agricultural crop.
CBD oils have become increasingly popular in lotions, tinctures and foods, but their legal status has been murky and the Food and Drug Administration has sent warning letters to some companies making health claims for CBD.
In a statement following Thursday’s bill signing in Washington, FDA Commissioner Scott Gottlieb restated his agency’s stance that CBD is a drug ingredient and therefore illegal to add to food or health products without approval from his agency.
“Selling unapproved products with unsubstantiated therapeutic claims is not only a violation of the law, but also can put patients at risk, as these products have not been proven to be safe or effective,” Gottlieb wrote.
CBD is a non-psychoactive compound found in hemp, a version of the cannabis plant that is low in THC, the part of cannabis that gives pot its high.
An FDA-approved drug for the treatment of seizures, Epidiolex, contains cannabis-derived CBD. GW Pharmaceuticals’ GWPH, +3.72% syrup became the first prescription drug derived from the cannabis plant in June.
The FDA statement also specified parts of hemp that are safe as food ingredients, but the CBD stance disappointed advocates. Courtney Moran, a lobbyist for Oregon hemp farmers, said she plans to work with U.S. Sen. Ron Wyden, an Oregon Democrat, to nudge the FDA toward greater acceptance of CBD.
“We do hope the FDA does clear a pathway for these products that have already hit store shelves and are out in the marketplace,” Moran said. She said it’s an “opportunity for industry to educate the FDA.”
The FDA statement said three ingredients derived from hemp — hulled hemp seeds, hemp seed protein and hemp seed oil — are safe as foods and won’t require additional approvals, as long as marketers do not make claims that they treat disease.
Hemp, like marijuana, already was legal in some states before Trump signed the farm bill. But now hemp farmers will be able to buy crop insurance, apply for loans and grants, and write off their business expenses on their taxes like any other farmer.
Food Irradiation Technology Not Widely Used With Fresh Produce, But It Could Be
December 7, 2018
By Stephen Kloosterman Contributing Editor
Food irradiation technology has been around for more than 50 years as a way to kill pathogens, although it is not widely used in the food processing industry.
Now, a growing firm called ScanTech Sciences is marketing its irradiation services for use with fresh produce.
ScanTech Sciences is building its first facility in McAllen, Texas’ Rio Grande Valley ECP Center. It opened for commercial operations during the summer 2018.
The facility can process between 120-160 cases of produce per minute, said Lindsay Eierman, ScanTech Sciences’ marketing manager. The company plans to open other facilities in ports of entry, such as New York/New Jersey and Nogales, Arizona, she said. Eventually, the company’s plans are to expand to areas such as of secondary import and export markets. Savannah, Georgia, Houston and California are among its targets.
University of Georgia Center for Food Safety Director Francisco Diez-Gonzalez spoke about the potential of the technique at the Southeast Regional Fruit and Vegetable Conference in January 2018.
“It’s been proven it can reduce the count of salmonella and listeria by more than 99.99 percent,” Diez-Gonzalez said. “It’s capable of killing viruses. It also helps to reduce microorganisms that could have an influence in spoilage.”
The technology, however, isn’t widespread in its use.
“Although the technology has been around for quite some time, it was not economical for use as a commercial application until the early 2000s,” Eierman said. In 2004, Australia shipped half a ton of irradiated mangoes to New Zealand, which was the first international use of food irradiation.
Food irradiation is approved by dozens of reputable organizations, including the U.S. Department of Agriculture, the Food and Drug Administration, the Centers for Disease Control, the American Medical Association and the United Nations World Health Organization, Eierman said. It’s also currently used as a post-harvest food process in more than 40 countries.
Room to grow
“There are two primary reasons that food irradiation is not more widely used,” Eierman said. “The first issue is intellectual property and investment. The technology is very complicated and requires expertise in nuclear engineering, mechanical engineering, and food science.”
Food irradiation can include the use of gamma rays, X-rays or electron beams, called e-beams. ScanTech Sciences’ patented form of e-beam food irradiation is Electronic Cold-Pasteurization, so-called because it allows product to be kept cold throughout the process. Not breaking the cold chain of storage is an added value for food processors.
The second reason food irradiation is uncommon, she said, is simply capacity. The technology is expensive, and Eierman said there have not been very many successful food irradiation ventures.
But that isn’t to say that food irradiation is rare.
Eierman said about a third of spices imported into the United States are irradiated. Many imported tropical fruits, such as guava, dragon fruit, persimmons and mangos, are irradiated. Also, much of the food consumed by NASA astronauts are irradiated to prevent sickness, according to the FDA’s website.
Eierman said food irradiation could be a good fit for processing fresh produce.
“Electronic Cold Pasteurization is a great solution for fruit, vegetables, herbs, spices and ready-to-eat (fresh-cut) commodities such as sliced apples,” she said. “It is particularly beneficial for commodities with short shelf life (such as berries or leafy greens), commodities with a high incidence of pests (such as peaches, which have the plum curculio), and commodities that are susceptible to contamination with pathogens (such as Listeria monocytogenes in cantaloupe or E. coli in lettuce).”
Irradiation is useful for not only for sanitizing foodstuffs but also eradicating pests.
One example of this is U.S. blueberry exports. Blueberry maggot fly larvae in the eastern U.S., and their presence in blueberries restricts exports of the berries to some countries trying to avoid infestation by the blueberry maggot fly. As certain chemical fumigants are phased out, irradiation is among tools being examined in a project led the U.S. Highbush Blueberry Council.
Eierman said her company’s technique of e-beam food irradiation could serve as a chemical-free alternative to methyl bromide fumigation, which remains in widespread use despite known downsides.
“Methyl bromide is a chemical fumigant that has been used for decades on imported and exported commodities as a pest control mechanism,” Eierman said. “Unfortunately, methyl bromide is a harmful ozone-depleting substance. The Montreal Protocol of 1987 was an international treaty that attempted to phase out the use of methyl bromide. However, methyl bromide remains in use because it is one of the few substances that provides effective pest control.”
Her company also hopes to combine its food irradiation services with integrated logistics, transportation and information services.
“These services reduce compliance costs associated with the Food Safety Modernization Act (FSMA),” she said. The Produce Safety Rule allows an exemption for produce that is going to a kill-step process. Electronic Cold-Pasteurization is a viable solution for meeting this exemption.
“ScanTech Sciences is eager to transform the food industry by providing safer, higher-quality produce,” Eierman said.
FDA certified
The U.S. Food and Drug Administration has evaluated the safety of irradiated food for more than 30 years and has found the process to be safe. FDA does, however, require irradiated foods bear the international symbol for irradiation. Look for the Radura symbol along with the statement “Treated with radiation” or “Treated by irradiation” on the food label. Bulk foods, such as fruits and vegetables, are required to be individually labeled or to have a label next to the sale container. The FDA does not require that individual ingredients in multi-ingredient foods (e.g., spices) be labeled.
Tags: food safety, listeria
YOU MIGHT ALSO LIKE
PMA names Impact Award winners
Taylor Farms voluntarily recalls salads over potential salmonella
Sanitation issues in packhouse led to cantaloupe listeria outbreak, FDA says
California Farm Linked To Romaine Lettuce E.coli Outbreak Recalls Additional Produce
To View The Video, Please Click Here
FDA believes market has been purged of contaminated romaine
A California farm that federal health officials traced to the recent E.coli outbreak from romaine lettuce has recalled additional produce “out of an abundance of caution,” the facility announced Thursday.
Adam Bros. Farming Inc. in Santa Maria has recalled red leaf lettuce, green leaf lettuce, and cauliflower that was harvest from Nov. 27 to Nov. 30.
Planning a trip to the sapphire seas of Aruba shouldn’t make you feel blue. Save time and money when you book air + hotel with JetBlue Vacations.
SOME ROMAINE LETTUCE SAFE TO EAT AGAIN, FDA SAYS
While none of the recalled products have tested positive for E. coli, and no illnesses associated with these produce items have been reported, the farm said: “Out of an abundance of caution, Adam Bros. Farming, Inc. is initiating this voluntary recall in cooperation with the FDA.”
“The recall was initiated after it was discovered that sediment from a reservoir near where the produce was grown tested positive for E. coli,” the farm explained.
Adam Bros. Farming Inc. added the recalled produce was “grown in particular fields” and does not involve all of its products.
“None of the filtered, treated water has tested positive for E. coli, all E. coli tests returning negative,” Adam Bros. Farming Inc. said, adding the bacteria “may cause a diarrheal illness from which most healthy adults can recover completely within a week. Some people can develop a form of kidney failure called Hemolytic Uremic Syndrome (HUS). HUS is most likely to occur in young children and the elderly. The condition can lead to serious kidney damage and even death.”
While Adam Bros. Farming Inc. has been linked to the food poisoning outbreak from romaine lettuce, federal health officials cautioned that other farms are likely involved in the E. coli outbreak and consumers should continue checking the label before purchasing romaine lettuce.
At least 59 people in 15 states have now been sickened by the tainted lettuce, the FDA said.
That said, regulators said they are fairly confident that the lettuce which first triggered the outbreak has been removed from the market. The FDA told consumers to avoid romaine lettuce just before Thanksgiving.
To learn more about the recent red leaf lettuce, green leaf lettuce and cauliflower recall -- like where these produce items were distributed -- click here.
The Associated Press contributed to this report.
Madeline Farber is a Reporter for Fox News. You can follow her on Twitter @MaddieFarberUDK.
FDA Looks At Labeling Standard, Plans To Allow Romaine Return
“We’re working with growers and distributors on labeling produce for location and harvest date and possibly other ways of informing consumers that the product is ‘post-purge,’”
Chris Koger November 23, 2018
In a trio of tweets Nov. 23, Food and Drug Administration Commissioner Scott Gottlieb referred to plans to allow romaine to return to the market, and a possible new labeling standard to aid in tracing products in future outbreaks.
Following Thanksgiving Day tweets that the FDA believes the E. coli-tainted romaine that led to a nationwide ban on the leafy green originated from California, Gottlieb said “the goal now is to withdraw the product that’s at risk of being contaminated from the market, and then re-stock the market.”
The Centers for Disease Control and Prevention and FDA announced the outbreak on Nov. 20, asking all levels of the supply chain to remove romaine from the market, and any that had been harvested but not shipped. Thirty-two people in the U.S. and 18 people in Canada became ill with E. coli from mid-October to early November.
In a Nov. 23 tweet, Gottlieb noted that romaine from different growing regions — Arizona and Florida — will soon be harvested.
“We’re working with growers and distributors on labeling produce for location and harvest date and possibly other ways of informing consumers that the product is ‘post-purge,’” he tweeted.
“We want to help unaffected growers get back into production and enable stores and consumers to re-stock,” Gottlieb tweeted. “One goal we’re seeking is to make this type of labeling the new standard rather than a short-term fix; as a way to improve identification and traceability in the system.”
On Thanksgiving, Gottlieb used Twitter to explain the decision to call for all romaine to be removed from the commerce stream.
“Some lettuce packing is labeled in a way that doesn’t make it clear where the product was grown,” he tweeted. “If you look at a package of lettuce, it’s most likely going to have the address of the company on the back; not the location of the growing fields.”
The United Fresh Produce Association on Nov. 20 advised companies to quickly comply and urged anyone contacted by regulatory agencies investigating the origin to help and make shipping records available. But it had also requested federal agencies to consider narrowing down the regions where romaine had been harvesting from when illnesses were reported, roughly mid- to late October.
“This is an extremely broad warning to consumers to not eat any type of romaine from any growing region,” according to a member alert from United Fresh. “Despite our urging that industry could clearly identify some sources of romaine coming onto the market as not related to the outbreak, CDC and FDA are also requesting the voluntarily withdrawal of romaine lettuce before it enters commerce.”
According to United Fresh, Yuma, Ariz., romaine had not commenced when the first illnesses were reported in mid-October.
Western Growers also asked regulators to use harvest and illness onset dates to target the possible growing region.
“ … It is important to acknowledge that a number of regions in current production were not harvesting or shipping romaine at the onset of the outbreak and, consequently, could not be the source of the specific E. coli strain identified in the illnesses,” according to a Western Growers statement on Nov. 21. “In light of this evidence, we urge the government’s health agencies to work with stakeholders to quickly narrow the scope of the investigation, and to remove these regions from the comprehensive advisory as soon as the safety of the public can be ensured.”
Related Topics: Outbreak E. coli Romaine United Fresh Western Growers